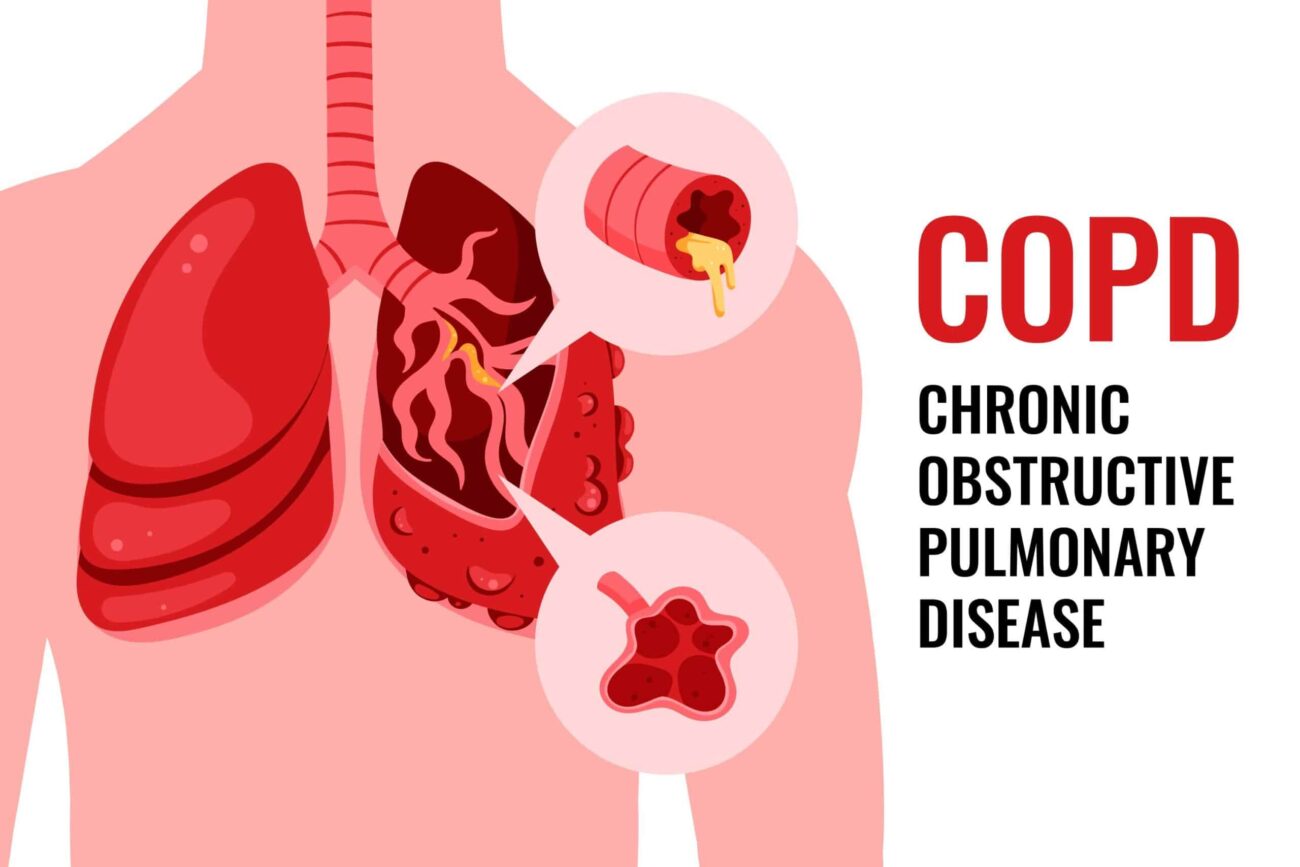
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
Chronic obstructive pulmonary disease (COPD) or chronic obstructive airway disease (COAD) are commonly used clinical terms for a group of pathological conditions in which there is chronic, partial or complete, obstruction to the airflow at any level from trachea to the smallest airways resulting in functional disability of the lungs i.e., these are diffuse lung diseases.
One of the most common etiologic factor (cause) for all forms of COPD is smoking.
The following entities are included in COPD:
- Chronic bronchitis
- Emphysema
- Bronchial asthma
Chronic bronchitis and emphysema are quite common and often occur together.
CHRONIC BRONCHITIS
Chronic bronchitis is a common condition defined clinically as persistent cough for a very long time. The cough is caused by over secretion of mucus. Oftenly, chronic bronchitis is associated with emphysema.
ETIOPATHOGENESIS (Etiology (cause) and pathogenesis ( how it is developed from the cause)
The two most important etiologic factors responsible for chronic bronchitis are: cigarette smoking and atmospheric pollution. Other factors are occupation, infection, familial and genetic factors.
1. Heavy smoking. – The most common cause of chronic bronchitis and emphysema is heavy smoking. Prolonged cigarette smoking act on the lungs in following ways-
- It impairs ciliary movement
- It inhibits the function of alveolar macrophages.
- It leads to hypertrophy and hyperplasia of mucus-secreting glands.
- It causes considerable obstruction of small airways.
- It stimulates the vagus and causes bronchoconstriction.
2. Atmospheric pollution- The development of chronic bronchitis is higher in industrialised urban areas where air is polluted. The atmospheric pollutants which increase the risk of developing chronic bronchitis are sulphur dioxide, nitrogen dioxide, particulate dust, and toxic fumes.
3. Occupation Workers engaged in certain occupations such as in cotton mills (byssinosis), plastic factories etc. are exposed to various organic or inorganic dusts which contribute to disabling chronic bronchitis in such individuals.
4. Infection Bacterial, viral and mycoplasmal infections.
5. Familial and genetic factors- There is less chance of familial tendency and genetic predisposition to develop disabling chronic bronchitis.
However, it is more likely that non-smoker family members who remain in the air-pollution of home are significantly exposed to smoke (passive smoking) and hence have increased blood levels of carbon monoxide.
MORPHOLOGIC FEATURES–
→The bronchial wall is thickened.
→ Mucus plugs develop in the bronchi and bronchioles.
CLINICAL FEATURES-
- Persistent cough with expectoration of long duration
- Recurrent respiratory infections
- Dyspnoea (shortness of breath).
- Chest X-ray shows enlarged heart with prominent vessels.
EMPHYSEMA
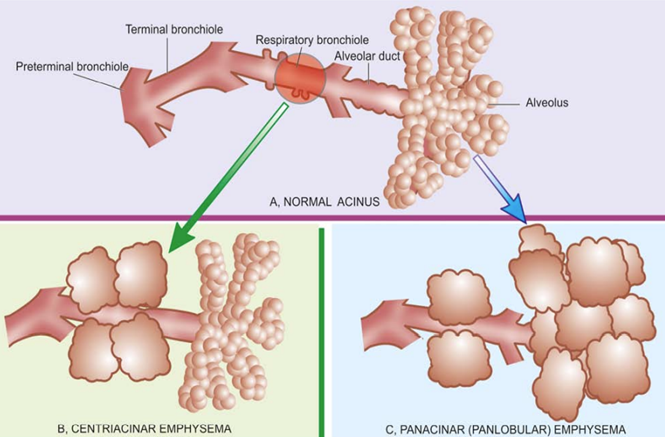
The WHO has defined pulmonary emphysema as combination of permanent dilatation of air spaces distal to the terminal bronchioles and the destruction of the walls of dilated air spaces.
ETIOLOGY
The two most common causes of emphysema are tobacco smoke and air pollutants.
Other causes are occupational exposure, infection, and familial and genetic influences.
PATHOGENESIS
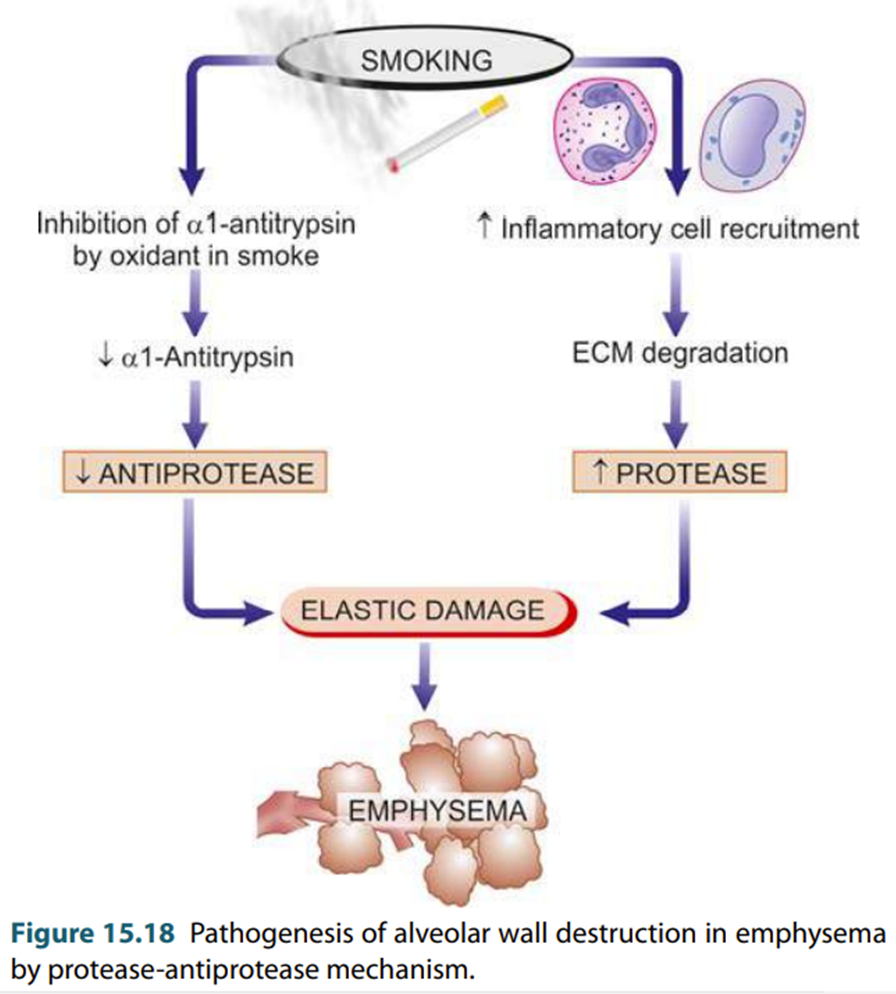
The mechanism of alveolar wall destruction in emphysema by elastolytic action is based on the imbalance between proteases (chiefly elastase) and anti-proteases (chiefly anti-elastase):
- By decreased anti-elastase activity due to deficiency of a-1 antitrypsin.
- By increased activity of elastase due to increased neutrophilic infiltration in the lungs causing excessive accumulation of neutrophil elastase.
There are enough evidences which suggest that smoking promotes emphysema by both decreasing the amount of anti-elastase as well as by increasing the elastolytic protease (elastase) in the lungs. These are as under:
1. Oxidant in cigarette smoke has inhibitory influence on a-1-antitrypsin, thus lowering the level of anti-elastase activity.
2. Smokers have up to ten times more phagocytes and neutrophils in their lungs than non-smokers; thus, they have very high elastase activity.
MORPHOLOGICAL FEATURES
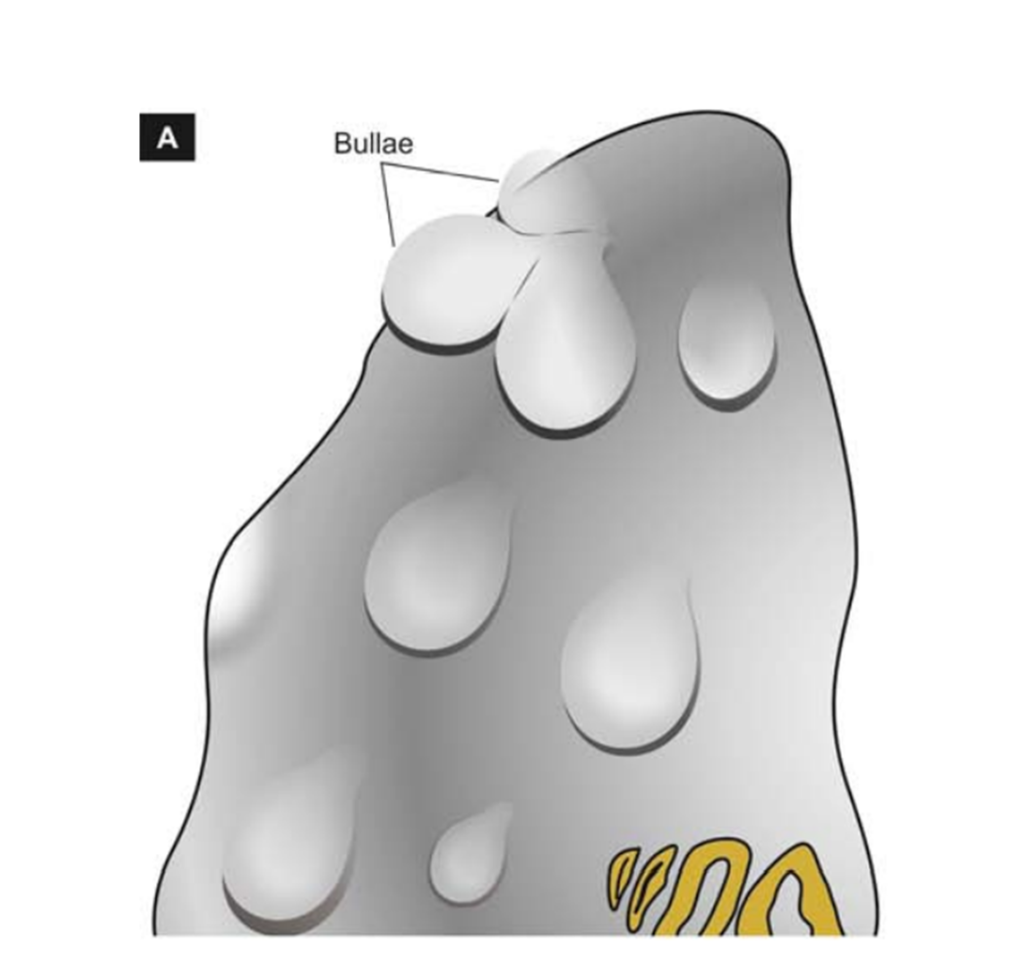
The lungs are voluminous (hyperinflated), pale with little blood. Mild cases show dilatation of air spaces visible with hand lens. Advanced cases show bullae and blebs bulging outwards from the surface of the lungs.
CLINICAL FEATURES
- Severe exertional dyspnoea.
- Patient is quite distressed
- Chest is barrel-shaped
- Cough with sputum.
- Weight loss.
- Right heart failure and hypercapneic respiratory failure are the terminal events.
- Chest X-ray shows small heart with hyperinflated lungs.
ASTHMA
Asthma is a disease of airways that is characterised by increased
responsiveness of the tracheobronchial tree to a variety of stimuli resulting in widespread
narrowing of the air passages.
Asthma is an episodic disease manifested clinically by paroxysms of
dyspnoea, cough, and wheezing.
ETIOPATHOGENESIS AND TYPES
Based on the stimuli initiating bronchial asthma, there are two types
of asthma: extrinsic (allergic, atopic) and intrinsic. There is also a third type of asthma called
mixed type in which patients have mixed
features of both.
1. Extrinsic (atopic, allergic) asthma-
⮚ This is the most common type of asthma.
⮚ It usually begins in childhood or in early adult life.
⮚ Most patients of this type of asthma have personal and/or family history of preceding allergic
diseases such as rhinitis, urticaria or infantile eczema.
⮚ Hypersensitivity to various ‘allergens’ is usually present. Most of these allergens include-
house dust, pollens, animal dander, moulds etc. Occupational asthma stimulated by fumes, gases and organic and chemical dusts is a variant of extrinsic asthma.
⮚ There is increased level of IgE in the serum.
2. Intrinsic (idiosyncratic, non-atopic) asthma-
⮚ This type of asthma develops later in adult life.
⮚ There is no personal or family history of allergy.
⮚ There is normal serum levels of IgE.
⮚ Most of these patients develop typical symptoms after an upper respiratory tract infection by
viruses. Associated nasal polypi and chronic bronchitis are commonly present.
⮚There are no recognisable factors (idiosyncratic) but about 10% of patients become hypersensitive
to drugs, mainly to small doses of aspirin (aspirin-sensitive asthma).
3. Mixed type- Many patients do not clearly fit into either of the above two categories and have mixed features of both.
MORPHOLOGICAL FEATURES
⮚ The lungs are overdistended due to over-inflation.
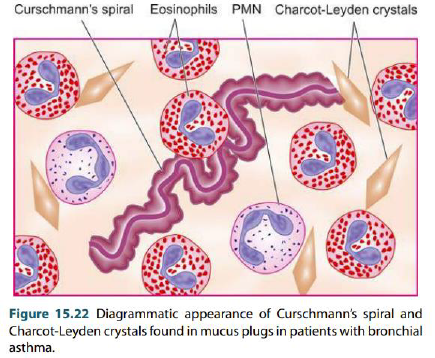
⮚ Occlusion of the bronchi and bronchioles by mucus plugs. The mucus plugs contain normal or degenerated respiratory epithelium forming twisted strips called Curschmann’s spirals.
⮚ The sputum usually contains numerous eosinophils and diamond-shaped crystals derived from eosinophils called Charcot-Leyden crystals.
⮚ The bronchial wall shows thickened basement membrane of the bronchial epithelium
⮚ Submucosal oedema
⮚ There is hypertrophy of submucosal glands as well as of the bronchial smooth muscle.
⮚ Bronchitis and emphysema may occur, especially in intrinsic asthma.
CLINICAL FEATURES
Paroxysms of dyspnoea, cough, and wheezing. Most attacks typically last for a few minutes to hours. When attacks occur continuously, it may result in more serious condition called status asthmaticus.
CLINICAL DIAGNOSIS
The clinical diagnosis is supported by demonstration of circulation eosinophilia (high eosinophile count) and sputum demonstration of Curschmann’s spirals and Charcot-Leyden crystals. More chronic cases may develop cor pulmonale.
REFERENCE
Harsh Mohan; Text book of Pathology; 6 th edition; India; Jaypee Publications; 2010