ACUTE RENAL FAILURE
Acute renal failure (ARF) is a syndrome characterised by rapid onset
of renal dysfunction (chiefly oliguria or anuria) and sudden increase
in metabolic waste-products (urea and creatinine) in the blood with
consequent development of uraemia.
ETIOPATHOGENESIS
The causes of ARF may be classified as-
1. Pre-renal causes- Pre-renal diseases are those which cause sudden decrease in blood flow to the nephron. Renal ischaemia ultimately results in functional disorders or depression of GFR, or both. causes of Renal ischaemia are- inadequate cardiac output and hypovolaemia or vascular disease, causing reduced perfusion of the kidneys.
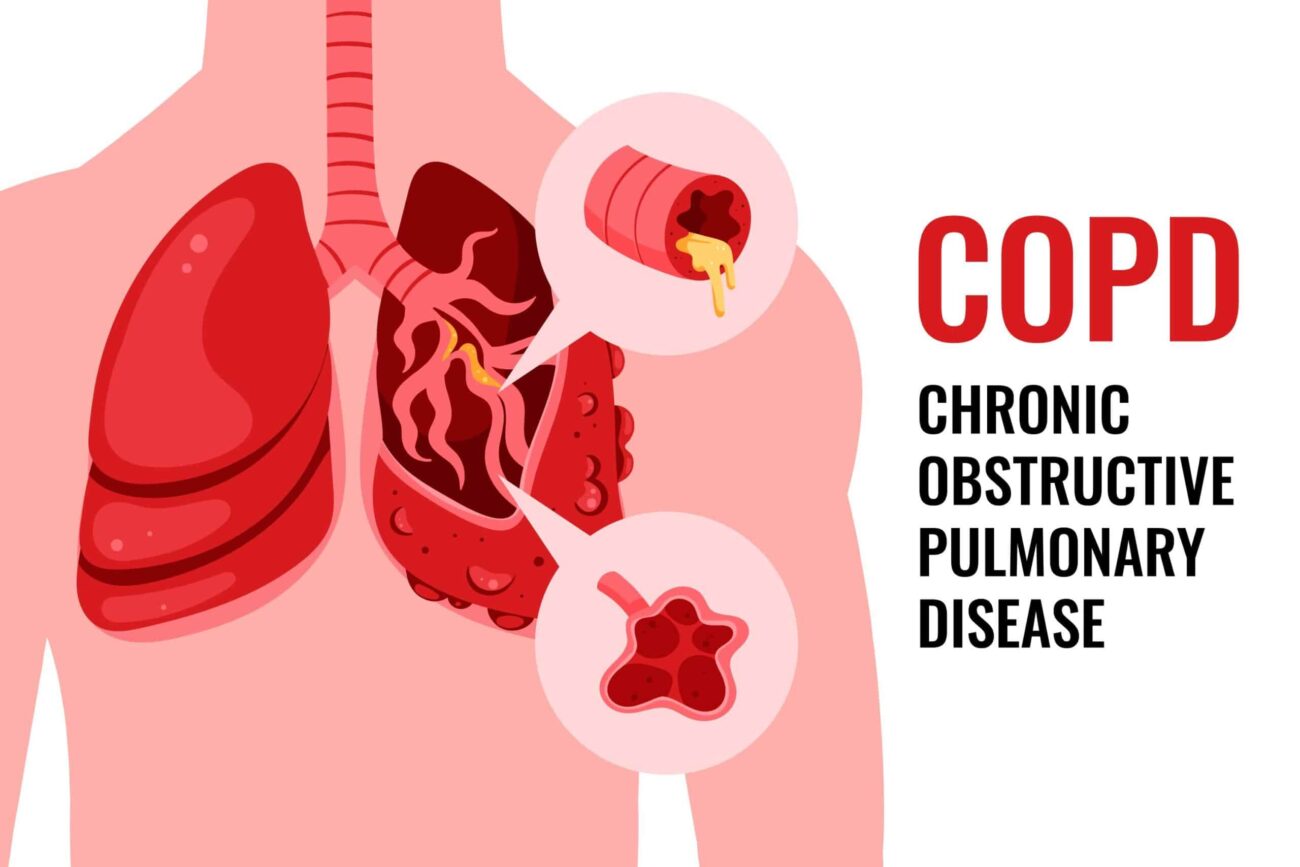
2. Intra-renal causes- Intra-renal disease is a disease of renal tissue itself. These include vascular disease of the arteries and arterioles within the kidney, diseases of glomeruli, acute tubular necrosis due to ischaemia, or the effect of a nephrotoxin, nephritis and pyelonephritis.
3. Post-renal causes- Post-renal disease is caused by obstruction to the flow of urine anywhere along the renal tract distal to the opening of the collecting ducts. This may be caused by a mass within the lumen or from wall of the tract, or from external compression anywhere along the lower urinary trac —ureter, bladder neck or urethra. It is important to note that Acute Renal Failure originating in pre- and post-renal disease eventually leads to intra-renal disease.
CLINICAL FEATURES
1. Syndrome of acute nephritis- This is most frequently associated glomerulonephritis. Renal dysfunction occurs due to extensive proliferation of epithelial cells in the glomeruli with consequent mild increase in glomerular permeability and decrease in GFR. The characteristic features are: mild proteinuria, haematuria, oedema and mild hypertension.
2. Pre-renal syndrome- The ARF occurring due to disorders in which neither the glomerulus nor the tubules are damaged, results in pre renal syndrome. This pattern occurs in marginal ischaemia. Due to depressed renal blood flow, there is decrease in GFR causing oliguria, azotaemia and fluid retention and oedema. Since the tubular cells are functioning normally, the nephron retains its ability to concentrate the glomerular filtrate according to the adaptive needs.
3. Syndrome accompanying tubular pathology- When the ARF is caused by destruction of the tubular cells, the disease typically progresses through 3 characteristic stages from oliguria to diuresis to recovery.
i) Oliguric phase: The oliguric phase lasts on an average from 7 to 10 days. It is characterised by urinary output of less than 400 ml per day. The decline in formation of the urine leads to accumulation of waste products in the blood.
ii) Diuretic phase: With the onset of healing of tubules, there is improvement in urinary output.
iii) Phase of recovery: Full recovery with healing of tubular epithelial cells occurs in about half the cases, while others terminate in death.
The process of healing may take up to one year.
CHRONIC RENAL FAILURE (CRF)
Chronic renal failure is a syndrome characterised by progressive and irreversible deterioration of renal function due to slow destruction of renal parenchyma, eventually terminating in death when enough nephrons have been damaged.Acidosis is the major problem in CRF along with azotaemia and uraemia.
ETIOPATHOGENESIS
All chronic nephropathies can lead to CRF.
The diseases leading to CRF can generally be classified into two major groups: those causing glomerular pathology, and those causing tubulointerstitial pathology
1. Diseases causing glomerular pathology
Glomerular destruction results in changes in filtration process and leads to development of the nephrotic syndrome characterised by proteinuria, hypoalbuminemia, and oedema.
The important examples of chronic glomerular diseases causing CRF-
i) Primary glomerular pathology: The major cause of CRF is chronic glomerulonephritis.
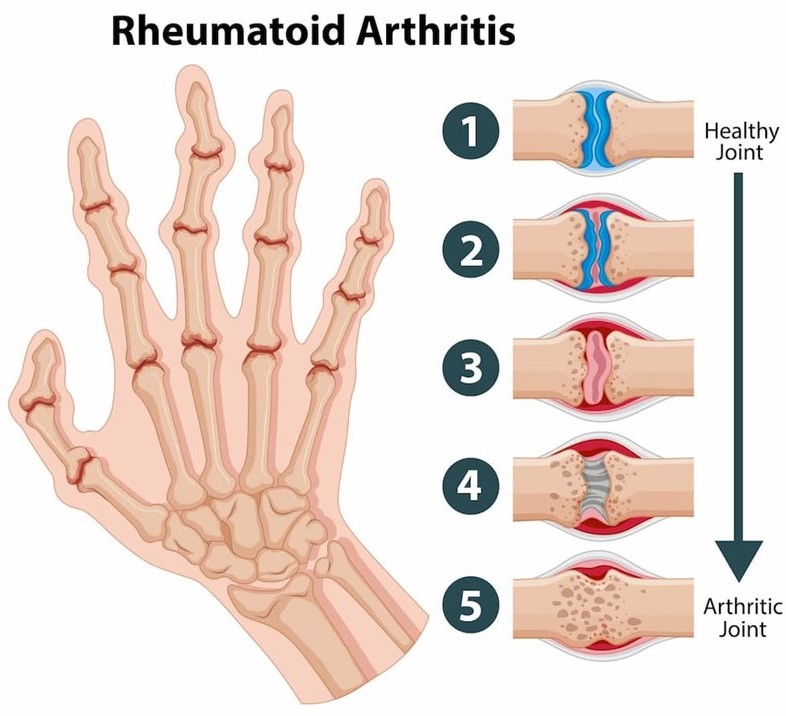
ii) Systemic glomerular pathology: Certain conditions originate outside the renal system but induce changes in the nephrons.
2. Diseases causing tubulointerstitial pathology
Damage to tubulointerstitial tissues results in alterations in reabsorption and secretion of important constituents leading to excretion of large volumes of dilute urine.
Tubulointerstitial diseases can be categorised according to initiating
etiology-
i) Vascular causes: Long-standing hypertension produces characteristic changes in renal arteries and arterioles that cause renal vascular occlusion terminating in ischaemia and necrosis of renal tissue.
ii) Infectious causes: Chronic pyelonephritis
iii) Toxic causes: High doses of analgesics, aspirin. Other substances
that can cause CRF are lead, cadmium and uranium.
iv) Obstructive causes: Chronic obstruction in the urinary tract leads to progressive damage to the nephron due to fluid backpressure.
examples are- stones, blood clots, tumours and enlarged prostate.
CRF evolves progressively through 4 stages:
1. Decreased renal reserve- At this stage, damage to renal parenchyma is marginal and the kidneys remain functional. The GFR is about 50% of normal, BUN and creatinine values are normal, and
the patients are usually asymptomatic.
2. Renal insufficiency- At this stage, about 75% of functional renal parenchyma has been destroyed. The GFR is about 25% of normal accompanied by elevation in BUN and serum creatinine. Polyuria and nocturia occur.
3. Renal failure- At this stage, about 90% of functional renal tissue has been destroyed. The GFR is approximately 10% of normal.
Tubular cells are essentially non-functional.
4. End-stage kidney (chronic kidney disease)- The GFR at this stage is less than 5% of normal and results in uraemic syndrome.
CLINICAL FEATURES
A. Primary uraemic (renal) manifestations-
Primary symptoms of uraemia develop when there is slow and progressive deterioration of renal function.
1. Metabolic acidosis- As a result of renal dysfunction, acid-base balance is progressively lost. Excess of hydrogen ions occurs, while bicarbonate level declines in the blood, resulting in metabolic acidosis.
2. Hyperkalaemia- A decreased GFR results in excessive accumulation of potassium in the blood since potassium is normally excreted mainly in the urine.
3. Sodium and water imbalance- As GFR declines, sodium and water cannot pass sufficiently into Bowman’s capsule leading to their retention.
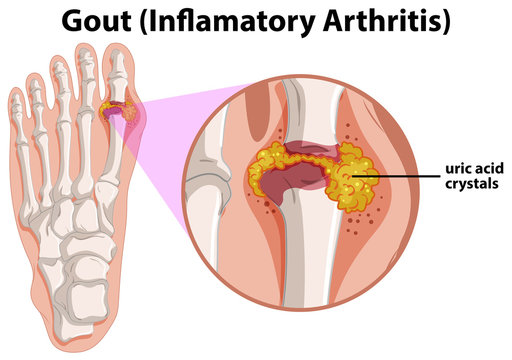
4. Hyperuricaemia- Decreased GFR results in excessive accumulation of uric acid in the blood. Uric acid crystals may be deposited in joints and soft tissues resulting in gout.
5. Azotaemia- The waste-products of protein metabolism fail to get excreted resulting in elevation in the blood levels of urea, creatinine, phenols.
B. Secondary uraemic (extra-renal) manifestations– Several extra nrenal systemic manifestations develop following fluid-electrolyte and acid-base imbalances. These include the following:
1. Decreased production of erythropoietin by diseased kidney results in decline in erythropoiesis and anaemia.
2. Integumentary system- Deposit of urinary pigment such as urochrome in the skin causes sallow-yellow colour.
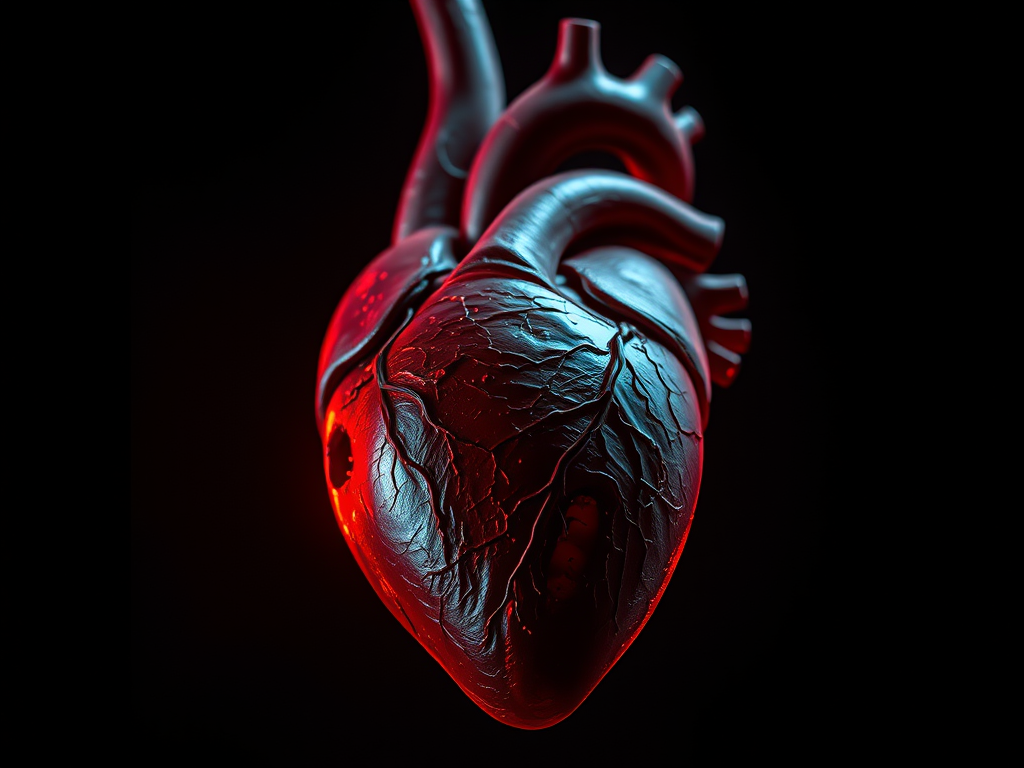
3. Cardiovascular system- Fluid retention secondarily causes increased workload on the heart and eventually congestive heart failure.
4. Digestive system- Azotaemia directly induces mucosal ulcerations in the lining of the stomach and intestines.
5. Skeletal system- Osteomalacia- It occurs from deficiency of a form of vitamin D which is normally activated by the kidney. Since vitamin D is essential for absorption of calcium, its deficiency results in
inadequate deposits of calcium in bone tissue.
REFERENCE
Harsh Mohan; Text book of Pathology; 6 th edition; India; Jaypee Publications; 2010