DEFINITION
Heart failure is defined as the pathophysiologic state in which impaired cardiac function is unable to maintain an adequate circulation for the metabolic needs of the tissues of the body. It may be acute or chronic. The term congestive heart failure (CHF) is used for the chronic form of heart failure in which the patient has evidence of congestion of peripheral circulation and of lungs.
ETIOLOGY
- INTRINSIC PUMP FAILURE- The most common and most important cause of heart failure is weakening of the ventricular muscle due to disease so that the heart fails to act as an efficient pump. The various diseases which may cause heart failure by this mechanism are as under:
i) Ischaemic heart disease
ii) Myocarditis
iii) Cardiomyopathies
iv) Metabolic disorders e.g., beriberi
v) Disorders of the rhythm e.g., atrial fibrillation and flutter. - INCREASED WORKLOAD ON THE HEART- Increased mechanical load on the heart results in increased myocardial demand resulting in myocardial failure. Increased load on the heart may be in the form of pressure load or volume load
i) Increased pressure load may occur in the following states:
a) Systemic and pulmonary arterial hypertension.
b) Valvular disease e.g., mitral stenosis, aortic stenosis, pulmonary
stenosis.
c) Chronic lung diseases.
ii) Increased volume load occurs when a ventricle is required to eject
more than normal volume of the blood resulting in cardiac failure.
This is seen in the following conditions:
a) Valvular insufficiency
b) Severe anaemia
c) Thyrotoxicosis
d) Arteriovenous shunts
e) Hypoxia due to lung diseases. - IMPAIRED FILLING OF CARDIAC CHAMBERS- Decreased cardiac output and cardiac failure may result from extracardiac causes or defect in filling of the heart:
a) Cardiac tamponade e.g., haemopericardium, hydropericardium
b) Constrictive pericarditis.
TYPES OF HEART FAILURE
I. ACUTE AND CHRONIC HEART FAILURE
Depending upon whether the heart failure develops rapidly or
slowly, it may be acute or chronic.
Acute heart failure
Sudden and rapid development of heart failure occurs in the following conditions:
i) Larger myocardial infarction
ii) Valve rupture
iii) Cardiac tamponade
iv) Massive pulmonary embolism
v) Acute viral myocarditis
vi) Acute bacterial toxaemia.
In acute heart failure, there is sudden reduction in cardiac output resulting in systemic hypotension, but oedema does not occur. Instead, a state of cardiogenic shock and cerebral hypoxia develops.
Chronic heart failure
More often, heart failure develops slowly as observed in the following states:
i) Myocardial ischaemia from atherosclerotic coronary artery disease
ii) Multivalvular heart disease
iii) Systemic arterial hypertension
iv) Chronic lung diseases resulting in hypoxia and pulmonary arterial
hypertension
v) Progression of acute into chronic failure.
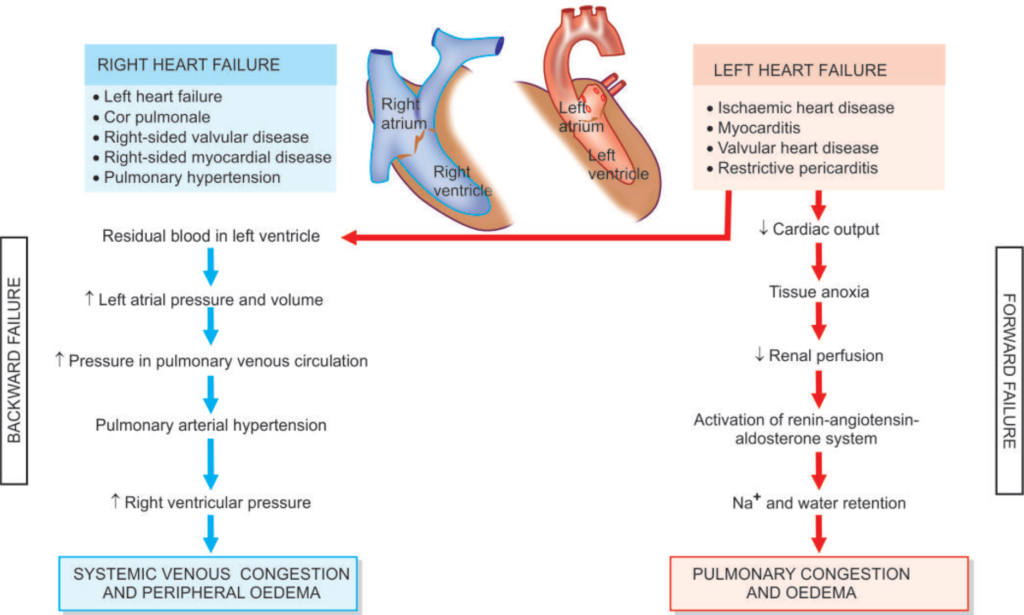
II. LEFT-SIDED AND RIGHT-SIDED HEART FAILURE
Though heart as an organ eventually fails as a whole, but functionally, the left and right heart act as independent units. Therefore, it is helpful to consider failure of the left and right heart separately.
Left-sided heart failure
It is initiated by stress to the left heart. The major causes are as
follows:
i) Systemic hypertension
ii) Mitral or aortic valve disease (stenosis)
iii) Ischaemic heart disease
iv) Myocardial diseases e.g., cardiomyopathies, myocarditis.
v) Restrictive pericarditis.
Left-sided heart failure causes decreased left ventricular output.
PATHOLOGICAL CHANGES
i) Pulmonary congestion and oedema causes dyspnoea
ii) Decreased left ventricular output causing hypoperfusion ischaemic acute tubular necrosis, in brain causing hypoxic encephalopathy, and in skeletal muscles causing muscular weakness and fatigue.
Right-sided heart failure
Left-sided heart failure causes decreased left ventricular output.
PATHOLOGICAL CHANGES
i) Pulmonary congestion and oedema causes dyspnoea
ii) Decreased left ventricular output causing hypoperfusion ischaemic
acute tubular necrosis, in brain causing hypoxic encephalopathy, and
in skeletal muscles causing muscular weakness and fatigue.
Right-sided heart failure
Right-sided heart failure occurs more often because of left-sided
heart failure. However, some conditions affect the right ventricle
primarily, producing right-sided heart failure. These are as follows:
i) Because of left ventricular failure.
ii) Cor pulmonale, in which right heart failure occurs due to intrinsic lung diseases
iii) Pulmonary or tricuspid valvular disease.
iv) Pulmonary hypertension.
v) Myocardial disease affecting the right heart.
vi) Congenital heart disease.
PATHOLOGIC CHANGES
Right-sided heart failure causes systemic and portal venous congestion, and reduced cardiac output.
Passive congestion of the liver, spleen, and kidneys.
In summary, the left heart failure manifests with features of pulmonary congestion and decreased left ventricular output, while the right heart failure presents with systemic venous congestion and involvement of the liver and spleen. CHF, however, combines the features of both left and right heart failure.
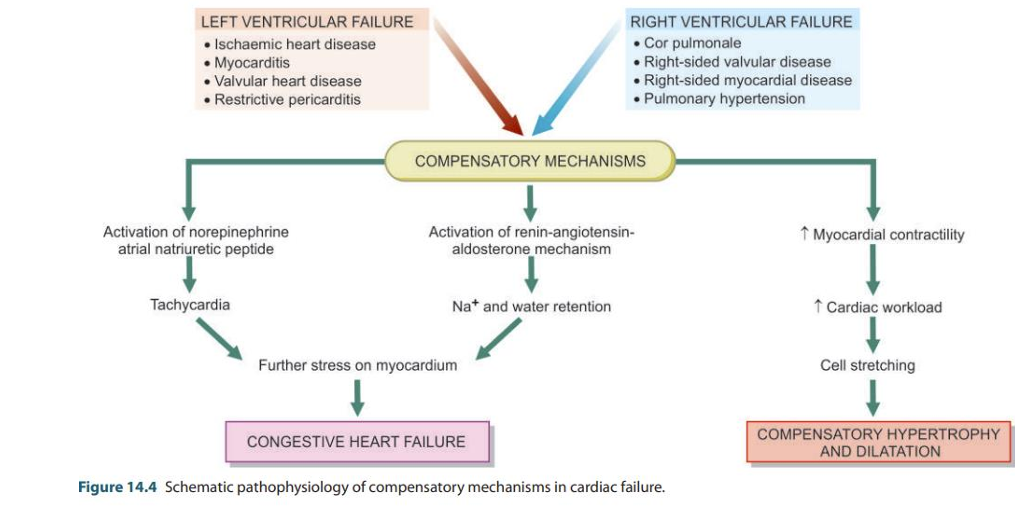
COMPENSATORY MECHANISMS:
Compensatory mechanisms to make adjustments so as to maintain adequate cardiac output:
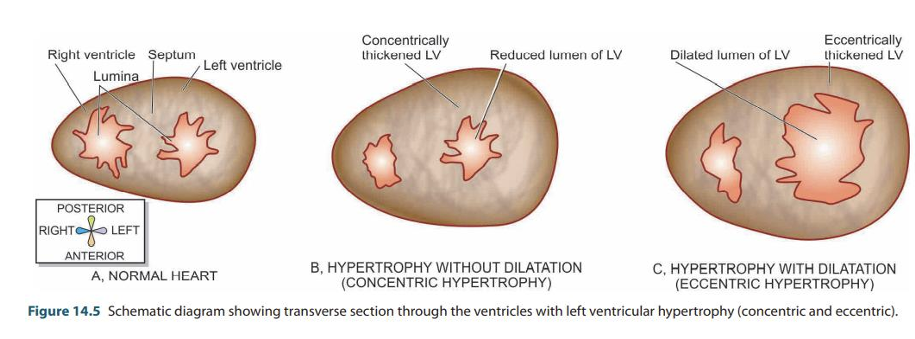
i) Compensatory enlargement in the form of cardiac hypertrophy, cardiac dilatation, or both.
ii) Tachycardia (i.e., increased heart rate) due to activation of neurohumoral system e.g., release of norepinephrine and atrial natriuretic peptide, activation of renin-angiotensin-aldosterone mechanism.
According to Starling’s law on pathophysiology of heart-
The failing dilated heart, to maintain cardiac performance, increases the myocardial contractility and thereby attempts to maintain stroke volume. dilatation of heart chambers decreases the force of contraction and leads to residual volume in the cardiac chambers causing volume overload resulting in cardiac failure that ends in death.
Reference
1. Harsh Mohan; Textbook of Pathology; 6th edition; India; Jaypee Publications; 2010.