Gout is a disorder of purine metabolism characterised by the following features, occurring singly or in combination:
1. Increased serum uric acid concentration (hyperuricaemia).
2. Recurrent attacks of acute arthritis
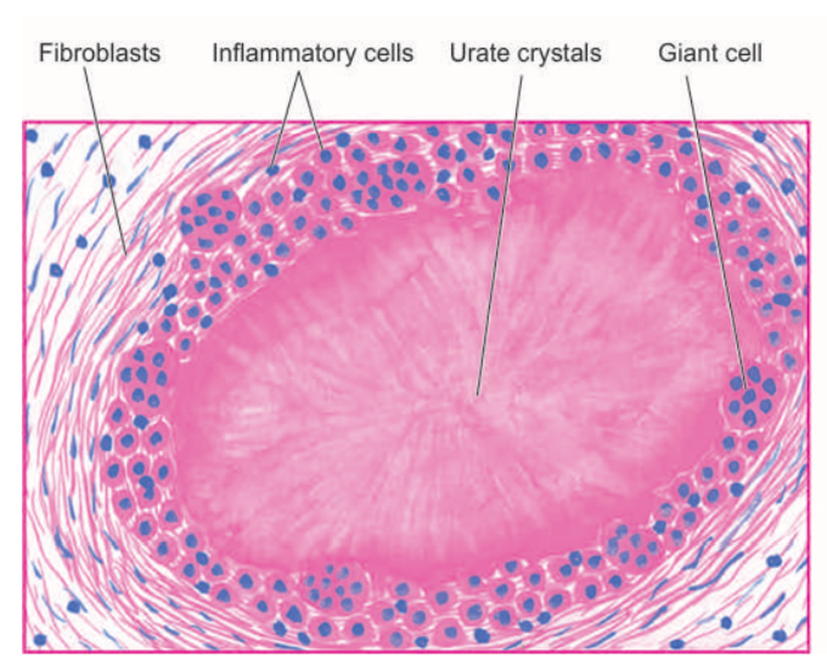
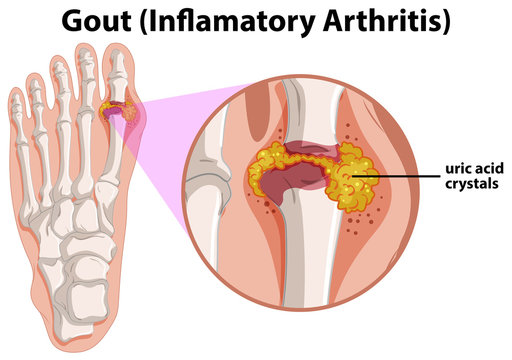
3. Aggregated deposits of monosodium urate monohydrate (tophi) in and around the joints of the extremities.
4. Renal disease involving interstitial tissue and blood vessels.
5. Uric acid renal calculi (kidney stones).
Gout comprises of 4 stages:
i. asymptomatic hyperuricaemia
ii. acute gouty arthritis
iii. asymptomatic intervals of intercritical periods
iv. chronic tophaceous stage
TYPES AND PATHOGENESIS
The fundamental biochemical hallmark of gout is hyperuricaemia.
Uric acid is the end product of purine metabolism in humans. The normal concentration of uric acid in the serum of adults is in the range of 3–7 mg/dl.
Hyperuricemia refers to an elevation in the serum uric acid concentration.
Gout is a metabolic disease associated with overproduction of uric acid. At the physiological pH, uric acid is found in a more soluble form as sodium urate. In severe hyperuricemia, crystals of sodium urate get deposited in the soft tissues, particularly in the joints. Such deposits are commonly known as tophi. This causes inflammation in the joints resulting in a painful gouty arthritis. Sodium urate and/or uric acid may also precipitate in kidneys and ureters that results in renal damage and stone formation.
Hyperuricaemia and gout may be classified into 2 types:
metabolic and renal, each of which may be primary or secondary.
Primary refers to cases in which the underlying biochemical defect causing hyperuricaemia is not known, while secondary denotes cases with known causes of hyperuricaemia.
1. Hyperuricaemia of metabolic origin– This group comprises about 10% cases of gout which are characterised by overproduction of uric acid. There is an accelerated rate of purine biosynthesis de novo.
It includes enzyme defects in purine metabolism which may be either of unknown cause or are inborn errors of metabolism.
- PRPP synthetase: In normal circumstances, PRPP synthetase is under feedback control by purine nucleotides (ADP and GDP). However, variant forms of PRPP synthetase—which are not subjected to feedback regulation—have been detected. This leads to the increased production of purines.
- PRPP glutamylamidotransferase : The lack of feedback control of this enzyme by purine nucleotides also leads to their elevated synthesis.
- Glucose 6-phosphatase deficiency: In type I glycogen storage disease (von Gierke’s), glucose 6-phosphate cannot be converted to glucose due to the deficiency of glucose 6-phosphatase. This leads to the increased utilization of glucose 6-phosphate by hexose monophosphate shunt (HMP shunt), resulting in elevated levels of ribose 5-phosphate and PRPP and, ultimately, purine overproduction.
2. Hyperuricaemia of renal origin– About 90% cases of gout are the result of reduced renal excretion of uric acid.
Altered renal excretion could be due to reduced glomerular filtration of uric acid, enhanced tubular reabsorption or decreased secretion.
The causes of gout of renal origin include diuretic therapy, drug-induced (e.g. aspirin, pyrazinamide, nicotinic acid, ethambutol and ethanol), adrenal insufficiency, starvation, diabetic ketosis, and disorders of parathyroid and thyroid.