The condition has high association with HLADR4 and HLADR1 and familial aggregation.
ETIOPATHOGENESIS
RA occurs in an immunogenetically predisposed individual because of microbial agents acting as trigger antigen.
The role of superantigens which are produced by several microorganisms with capacity to bind to HLADR molecules (MHCII region) has also emerged.
I. Immunologic derangements – There is a role of immune processes, particularly autoimmune phenomenon, in the development of RA. These include the following:
1. Detection of circulating autoantibody called rheumatoid factor (RF) against Fc portion of IgG.
2. The presence of antigenantibody complexes (IgGRFcomplexes) in the circulation as well as in the synovial fluid.
3. The presence of other autoantibodies such as antinuclear factor (ANF), antibodies to collagen type II, and antibodies to cytoskeleton.
4. Activation of cellmediated immunity as observed by presence of numerous inflammatory cells in the synovium, chiefly CD4+ T lymphocytes and some macrophages.
II. Trigger events: The trigger events initiate the destruction of articular cartilage. These include:
1. The existence of an infectious agent such as mycoplasma, EpsteinBarr virus (EBV), cytomegalovirus (CMV) or rubella virus, either locally in the synovial fluid or systemic infection some time prior to the attack of RA.
2. The possible role of HLADR4 and HLADR1 in initiation of immunologic damage.
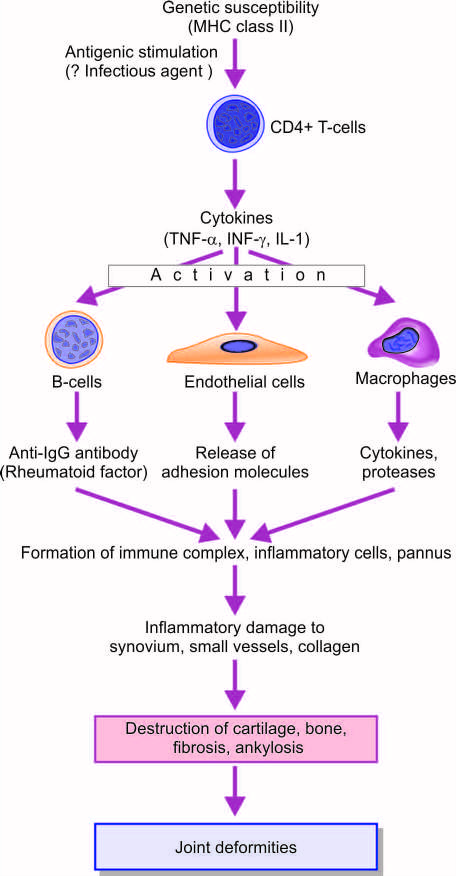
The proposed events in immunopathogenesis of RA are as under (see given figure):
i) In response to antigenic exposure (e.g., infectious agent) a genetically predisposed individual (HLADR), CD4+T cells activated.
ii) These cells elaborate cytokines- tumour necrosis factor (TNF) alpha, interferon (IF) gamma, interleukin (IL)1 and IL6.
iii) These cytokines activate endothelial cells, B lymphocytes and macrophages.
v) IgG and IgM immune complexes trigger inflammatory damage to the synovium, small blood vessels and collagen.
vi) Activated endothelial cells express adhesion molecules which stimulate collection of inflammatory cells.
vii) Activation of macrophages releases more cytokines which use damage to joint tissues and vascularisation of cartilage termed pannus formation.
viii) These events gradually damage and destruction of bone and cartilage. These are followed by fibrosis and ankylosis producing joint deformities.
MORPHOLOGIC FEATURES
The pathologic lesions are found mainly in the joints and tendons, and less often, extraarticular lesions are encountered.
ARTICULAR LESIONS
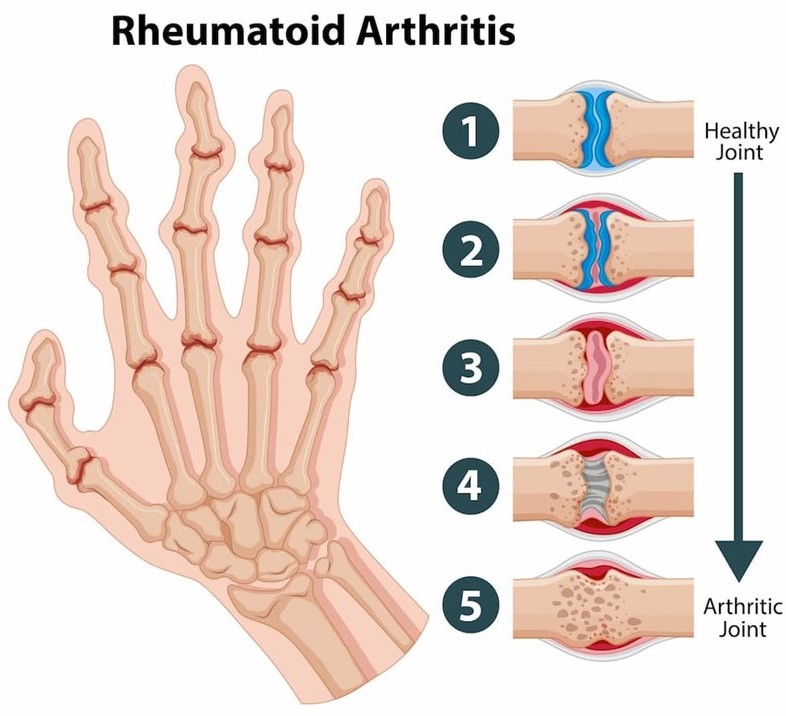
RA involves first the small joints of hands and feet and then symmetrically affects the joints of wrists, elbows, ankles, and knees. The proximal interphalangeal and metacarpophalangeal joints are affected most severely. Frequently cervical spine is involved but lumbar spine is spared.
Histologically, the characteristic feature is proliferative synovitis with formation of pannus. The microscopic changes are as under:
1. Numerous folds of large villi of synovium.
2. Marked thickening of the synovial membrane due to oedema, congestion.
3. Intense inflammatory cells in the synovial membrane- lymphocytes, plasma cells and some macrophages
4. Fibrinoid necrosis and fibrin deposition.
EXTRA-ARTICULAR LESIONS
Nonspecific inflammatory changes are seen in the blood vessels (acute vasculitis), lungs, pleura, pericardium, myocardium, lymph nodes, peripheral nerves, and eyes.
But one of the characteristic extraarticular manifestation of RA is occurrence of rheumatoid nodules in the skin (located mainly in elbows and fingers). These nodules may be found in visceral organs.
REFERENCE
Harsh Mohan; Text book of Pathology; 6 th edition; India; Jaypee Publications; 2010