ENDOCRINE PANCREAS
The human pancreas, though anatomically a single organ, histologically and functionally, has 2 distinct parts—the exocrine and endocrine. Exocrine part produces pancreatic juices containing digestive enzymes and releases it into ducts. Endocrine gland produces hormones and releases it directly into bloodstream.
NORMAL STRUCTURE of ENDOCRINE PANCREAS
The endocrine pancreas consists of collections of cells called islets of Langerhans found scattered within the pancreatic lobules.
The islet cell tissue is greatly concentrated in the tail than in the head or body of the pancreas. Islets do not have duct system and they drain their secretory products directly into the circulation.
Different types of Islet cells are-
A. Major cell types:
1. Beta (β) or B cells -secrete insulin that lowers blood glucose levels
2. Alpha (α) or A cells – secrete glucagon that raises blood glucose levels.
3. Delta (δ) or D cells – secrete somatostatin which suppresses both insulin and glucagon release.
4. Pancreatic polypeptide (PP) cells or F cells – secrete pancreatic polypeptide having some gastrointestinal effects.
B. Minor cell types:
1. D1 cells- produce vasoactive intestinal peptide (VIP) which induces glycogenolysis
2. Enterochromaffin cells- synthesise serotonin which in pancreatic tumours may induce carcinoid syndrome.
DIABETES MELLITUS
DEFINITION
Diabetes mellitus (DM) is defined as a metabolic disorder characterised by common feature of chronic hyperglycaemia with disturbance of carbohydrate, fat, and protein metabolism.
CLASSIFICATION AND ETIOLOGY
Classification of DM based on etiology divides it into two broad categories—type 1 and type 2; besides there are a specific etiologic type, and gestational DM.
TYPE 1 DM- It was previously termed as juvenile-onset diabetes (JOD) due to its occurrence in younger age, and was called insulin-dependent DM (IDDM) because it was known that these patients have absolute requirement for insulin replacement as treatment.
Based on underlying etiology, type 1 DM is further divided into 2 subtypes:
Subtype 1A (immune-mediated)- Autoimmune destruction of β-cells which usually leads to insulin deficiency.
Subtype 1B (idiopathic)- Insulin deficiency with tendency to develop ketosis but these patients are negative for autoimmune markers. (Unknown cause)
TYPE 2 DM- This type comprises about 80% cases of DM. It was previously called maturity-onset diabetes, or non-insulin dependent diabetes mellitus (NIDDM) of obese and nonobese type. Although type 2 DM predominantly affects older individuals, it is now known that it also occurs in obese adolescent children; hence the term MOD for it is inappropriate. Moreover, many type 2 DM patients also require insulin therapy to control hyperglycaemia or to prevent ketosis and thus are not truly non-insulin dependent.
OTHER TYPES OF DM
Maturity-Onset Diabetes of The Young (MODY)-It has autosomal dominant inheritance, early onset of hyperglycaemia and impaired insulin secretion.
GESTATIONAL DM- Some pregnant women develop DM due to metabolic changes during pregnancy. Although they revert to normal glucose levels after delivery, these women are prone to develop DM later in their life.
Major risk factors for type 2 diabetes mellitus
1. Family history
2. Obesity
3. Habitual physical inactivity
4. History of gestational DM or delivery of baby heavier than 4 kg
5. Hypertension
6. Dyslipidaemia (HDL level < 35 mg/dl or triglycerides > 250 mg/d
7. Polycystic ovary disease
8. History of vascular disease
PATHOGENESIS OF TYPE 1 DM
The basic phenomenon in type 1 DM is destruction of β-cell mass leading to absolute insulin deficiency.
Pathogenesis of type 1B DM is idiopathic and pathogenesis of type 1A DM is immune-mediated.
Pathogenesis of Type1 DM is based on following mechanisms-
- Genetic susceptibility-
Type 1A DM involves inheritance of multiple genes that confer susceptibility to the disorder:
i) It is observed in identical twins that if one twin has type 1A DM, there is about 50% chance of the second twin developing. This means that some additional modifying factors are involved in development of DM in these cases.
ii) About half the cases with genetic predisposition to type 1A DM have the susceptibility gene located in the HLA region of chromosome 6.
2. Autoimmunity-
i) Presence of islet cell antibodies against GAD (glutamic acid decarboxylase), insulin etc.
ii) Occurrence of lymphocytic infiltrate in and around the pancreatic islets termed insulitis. It chiefly consists of CD8+ T lymphocytes.
iii) Selective destruction of β-cells while other islet cell types remain unaffected. This is mediated by T-cell mediated cytotoxicity or by apoptosis.
iv) Association of type 1A DM with other autoimmune diseases in some cases such as Graves’ disease, Addison’s disease, Hashimoto’s thyroiditis, pernicious anaemia.
3. Environmental factors-
i) Certain viral infections preceding the onset of disease e.g. mumps, measles, coxsackie B virus, cytomegalovirus and infectious mononucleosis.
ii) Induction of type 1A DM by certain chemicals e.g. alloxan, streptozotocin and pentamidine.
iii) Geographic and seasonal variations in occurrence of type 1A DM suggest some common environmental factors.
iv) Possible relationship of early exposure to bovine milk proteins and occurrence of autoimmune process in type 1A DM.

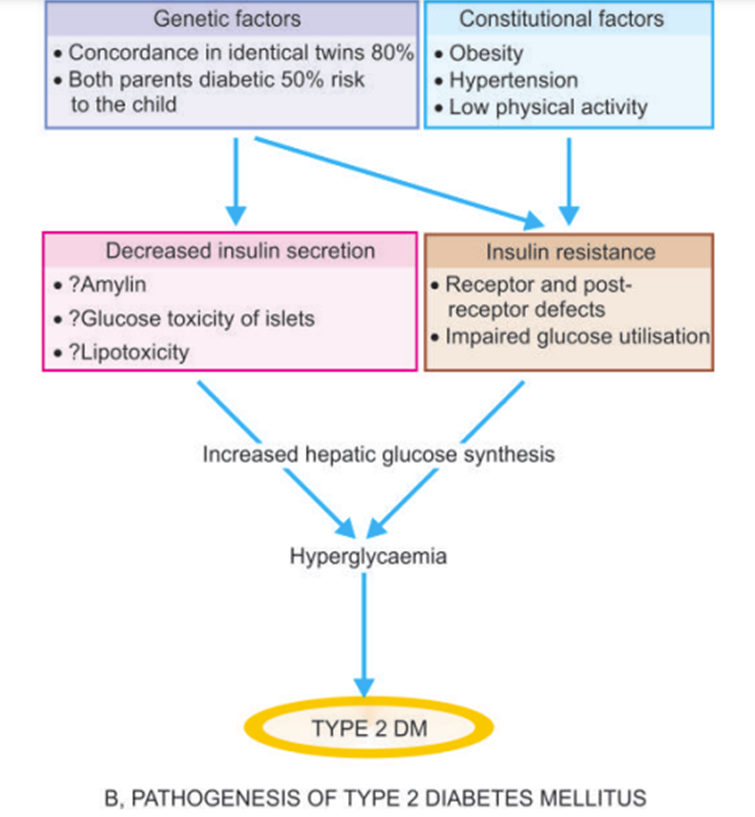
PATHOGENESIS OF TYPE 2 DM
The basic metabolic defect in type 2 DM is either a delayed insulin secretion relative to glucose load (impaired insulin secretion), or the peripheral tissues are unable to respond to insulin (insulin resistance).
Autoimmune phenomena and HLA are not associated with TYPE 2 DM.
- Genetic factors– Genetic component has a stronger basis for type 2 DM than type 1A DM. Although no definite genes have been identified, multifactorial inheritance is the most important factor in development of type 2 DM:
- There is approximately 80% chance of developing diabetes in the other identical twin if one twin has the disease.
- A person with one parent having type 2 DM is at an increased risk of getting diabetes, but if both parents have type 2 DM the risk in the offspring rises to 40%.
- Constitutional factors- Certain environmental factors such as obesity, hypertension, and level of physical activity play contributory role in the development of disease.
- Insulin resistance- One of the most prominent metabolic features of type 2 DM is the lack of responsiveness of peripheral tissues to insulin, especially of the skeletal muscle and liver. Obesity is strongly associated with insulin resistance.
Mechanism of hyperglycaemia:
i) Resistance to action of insulin impairs glucose utilisation and hence hyperglycaemia.
i) There is increased hepatic synthesis of glucose.
iii) Hyperglycaemia in obesity is related to high levels of free fatty acids and cytokines that affect peripheral tissue sensitivity to respond to insulin.
Underlying defects causing insulin resistance-
a) Polymorphism in various post-receptor intracellular signal pathway molecules.
b) Elevated free fatty acids seen in obesity result in impaired glucose utilisation in the skeletal muscle, increased hepatic synthesis of glucose, and impaired β-cell function.
c) Insulin resistance syndrome is a complex of clinical features that occurs due to insulin resistance causes hyperglycaemia and compensatory hyperinsulinaemia.
4. Impaired insulin secretion- In type 2 DM, insulin resistance and insulin secretion are interlinked:
i) Early in the course of disease, in response to insulin resistance there is compensatory increased secretion of insulin (hyperinsulinaemia) to maintain normal blood glucose level.
ii) Eventually, however, there is failure of β-cell function to secrete adequate insulin.
Reasons for fall in insulin secretion-
a) Islet amyloid polypeptide (amylin) forms fibrillar protein deposits in pancreatic islets impairs the function of β -cells.
b) Metabolic environment of chronic hyperglycaemia surrounding the islets (glucose toxicity) paradoxically impair islet cell function.
c) Elevated free fatty acid levels (lipotoxicity) worsen islet cell function.
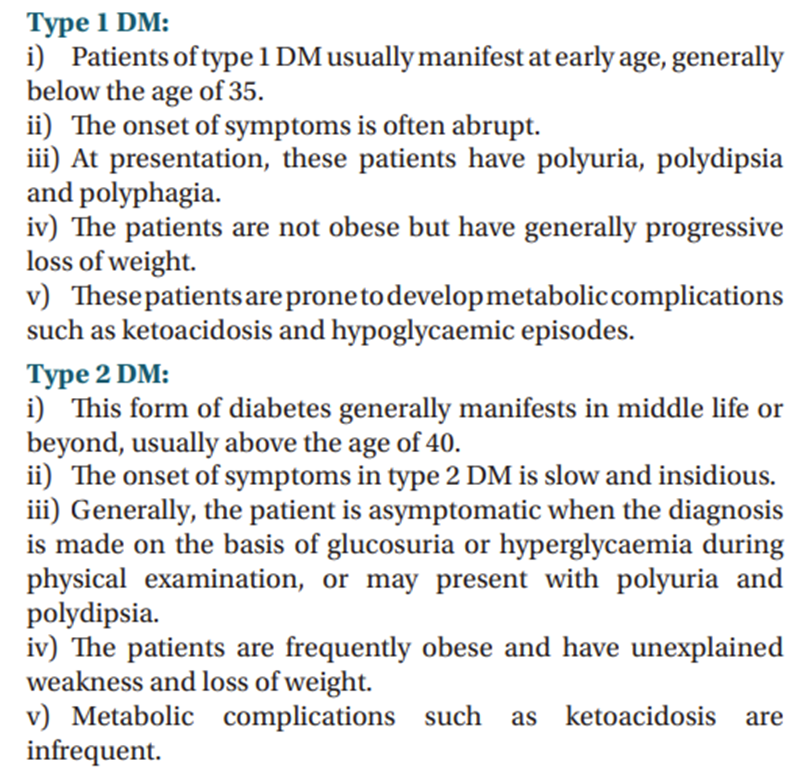
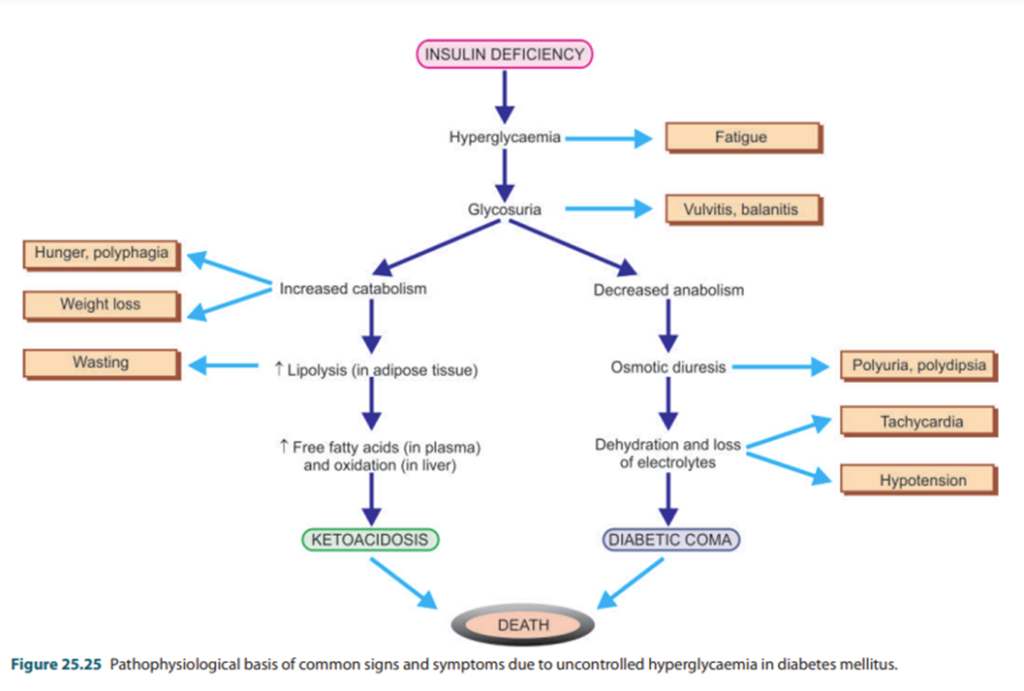
CLINICAL FEATURES
Hyperglycaemia in DM does not cause a single disease but is associated with numerous diseases and symptoms and complications as given below (can be used for additional points for difference between Type 1 and Type 2 diabetes).
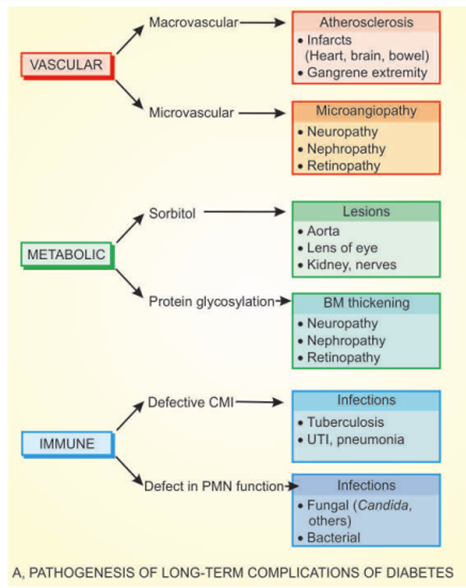
PATHOGENESIS OF COMPLICATIONS
In both type 1 and 2 DM, severity and chronicity of hyperglycaemia forms the main mechanism for ‘microvascular complications’ (e.g., retinopathy, nephropathy, neuropathy); therefore, control of blood glucose level constitutes the mainstay of treatment for minimising development of these complications.
Longstanding cases of type 2 DM, however, in addition, frequently develop ‘macrovascular complications’ (e.g., atherosclerosis, coronary artery disease, peripheral vascular disease, cerebrovascular disease).
COMPLICATIONS OF DIABETES
REFERENCE
Harsh Mohan; Text book of Pathology; 6 th edition; India; Jaypee Publications; 2010